During a heart transplant, a specialized team removes your diseased heart and replaces it with a healthy heart from a donor. The procedure is a major surgery that involves risk. But with close monitoring and the supportive care of an experienced team, many people are able to lead a relatively normal life after heart transplant.
A heart transplant is typically the last option for heart failure treatment when medicine, lifestyle modifications, and other treatments can no longer manage the condition and prevent it from getting worse. If other forms of treatment aren't preventing your symptoms from worsening, a heart transplant might be for you.
National Leaders in Heart Transplantation
Temple has some of the best heart transplant outcomes in the Philadelphia region and is among the best in the country. Our physicians manage some of the most complex patients including those who need multiple organ transplantation (heart-lung, heart-liver). The benefits of our expertise include:
- 85.0% of our patients who receive a heart transplant are living with a functioning heart 1 year after their procedure.
- Our expertise in donor heart assessment results in faster time to transplant. 70.9% of Temple patients received a donor heart within 1 year. The national average is 55.2%.
- Transplant eligibility criteria here are broader than most. Patients who have been turned down for transplantation at other centers may be eligible at Temple.
Learn more about how Temple’s Heart Transplant Program is setting the standard for excellence.
If you’re considered a candidate for heart transplant at Temple, you will be placed on a waiting list for a donor heart. Once your heart transplant has been performed, a team of heart transplant specialists will monitor your care throughout your life.
Getting on the Heart Transplant Waiting List
Temple’s Heart Transplant Program has a reputation for shorter time to transplant for waitlist candidates. Part of our success is due to our expanded transplant criteria, which allows more patients to qualify for this life-saving surgery.
To get on the waiting list, you must have an appointment with Temple advanced heart failure specialist. Our heart failure team will perform an evaluation. This includes a physical exam, diagnostic tests and a psychological assessment, which help us determine if you’re a good heart transplant candidate.
Temple’s comprehensive pre-transplant evaluation is an important step in the process, as there is a high demand for transplant organs and a relatively low supply.
Our recently expanded heart transplant criteria allows us to consider patients who:
- Are up to age 74 (age 70 at other centers)
- Have a BMI up to 35
- Have had cancer within the past 5 years
- Are HIV positive
- Have other significant conditions
- Have had multiple sternotomies
Once you’re added to the waiting list, you may get an organ that day or you may wait years. This depends on how well you match with a donor and how sick you are.
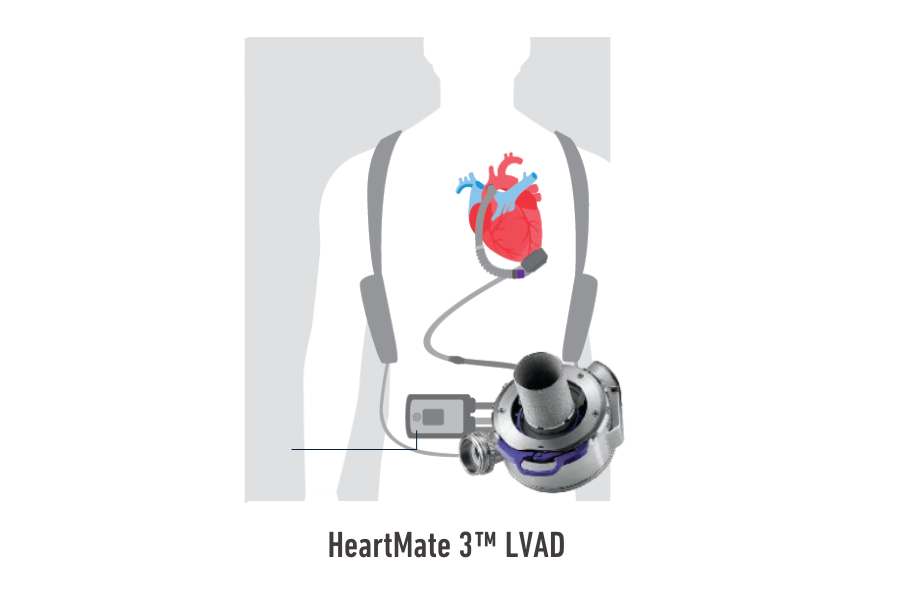
If you require biventricular support while you wait for a donor heart, Temple surgeons and advanced heart failure specialists work with you to provide support and consider options, including heart pumps (also called mechanical circulatory support or VAD) or a total artificial heart.