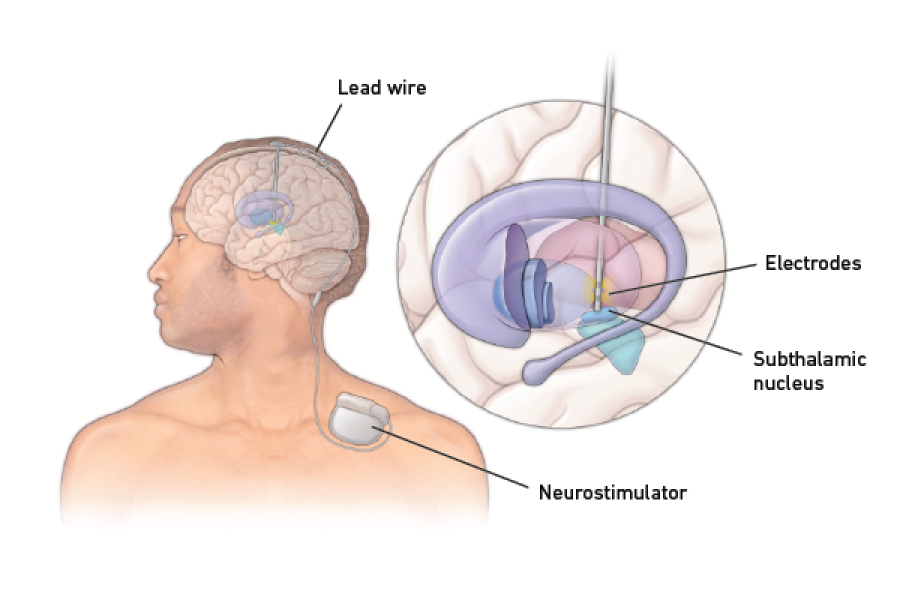
Once it's in place, the DBS system acts as a "brain pacemaker." It delivers a small electrical stimulation calming the abnormal rhythms in the brain that can cause tremor, stiffness, slowness, twisting or other symptoms of Parkinson’s disease and other movement disorders. For epilepsy, DBS is thought to work by calming and regulating the brain. This results in fewer and less severe seizures.
Your physician can work with you to adjust the stimulation, improving results over time. Some newer DBS technology can even personalize itself, automatically adjusting stimulation to a patient’s individual symptoms.
You can learn more about the DBS process by reviewing our frequently asked questions.
Am I a Good Candidate for Deep Brain Stimulation?
Some patients get more benefit from DBS than others. Doctors will evaluate you to determine if DBS is right for you.
You may be a candidate for DBS if:
- You have Parkinson’s disease and are bothered by movement symptoms like tremor, stiffness, slowness, or dyskinesia (rapid, uncontrolled movements). DBS can also help if you want to reduce Parkinson's medications, or if you're bothered by medication side effects.
- You have essential tremor that is not controlled with medications.
- You have dystonia (including torticollis) that is not controlled with medications.
- You have epilepsy and are still having seizures despite being on medication.
- You have severe OCD or Tourette’s syndrome not controlled by medications or psychotherapy.
Learn more about the evaluation process or, request an appointment with a Temple Health physician to find out if you are a candidate for DBS.
What Are the Benefits of Deep Brain Stimulation?
- Patients with Parkinson’s disease usually see 60% to 90% improvement in their tremor, and also see improvement in stiffness and slowness. Most have fewer medication side effects, and fewer "ups and downs" of symptom control than with medication alone. Some patients may see improved walking, pain or sleep.
- Patients with essential tremor usually see 60% to 90% improvement in their tremor, and greater ability to do daily tasks like eating, dressing, and writing.
- Patients with dystonia usually see improvement in twisting and other movements, along with reduced pain.
- Patients with epilepsy may see their number of seizures cut by half or more.
Why Temple Health for Deep Brain Stimulation?
Temple's Neurosciences Center provides state-of-the-art care for complex neurologic diseases. Our team of neurologists, neurosurgeons, neuropsychologists, physical and occupational therapists, speech therapists, and other professionals works closely with each patient to provide personalized care and therapies tailored to their individual needs. We have deep connections with the Philadelphia community and surrounding areas, and build close relationships with patients. Our expertise allows us to treat all types of movement disorders, from simple to very complex.
Ready for an Appointment?
Find a doctor near you, request an appointment, or call 800-TEMPLE-MED (866-597-3109) today.