Back to top >
How to Prepare for Surgery
Preparing for surgery requires lifestyle changes physically, emotionally, mentally and financially. As you are preparing, take the following into consideration:
Check with Your Insurance Company
Most insurance plans cover Roux-en-Y gastric bypass if you meet the qualifications. Before your procedure, check with your insurance company to make sure you understand your coverage, including any co-pays or out-of-network considerations. Temple will help you with any pre-authorizations or required approvals.
Schedule Any Required Tests
Work with your bariatric team to complete any tests required prior to your procedure. Your bariatric surgeon will determine what tests you need based on insurance requirements and an evaluation of your overall health. These tests may include blood work and chest X-ray as well as an evaluation of your heart and gastrointestinal (GI) system.
Re-Think Your Relationship with Food
You’ll meet with a Temple dietitian in the months before your procedure to evaluate your nutrition and overall eating patterns. You'll work together to create healthier habits and prepare for long-term success after your surgery. Losing weight before your gastric bypass surgery will help you recover faster.
Your dietitian will also need to provide required paperwork to your insurance company to show that you’re committed to a successful procedure.
Move As Much As Possible
Successful long-term weight loss is a complex process that includes many different factors of your well-being. One of those factors is physical exercise. Even if you have not exercised in a long time, it’s important to move every single day before your procedure, and after you start your recovery process. Commit to moving just a little bit every day, even if it’s just a few steps.
If You Smoke, Now’s the Time to Quit
Smoking increases your risk of complications during and after gastric bypass surgery. If you smoke cigarettes or use any type of tobacco or nicotine product, talk to your doctor about strategies for quitting prior to your procedure.
Read Up and Ask Questions
During your initial consultation, you’ll receive a packet to take home and read. But don’t stop there. Conduct your own research about Roux-en-Y gastric bypass, talk to others who have been through the procedure, and ask your Temple weight-loss team as many questions as possible. You are the center of your own health care team, so make sure you are well-informed.
Download our bariatric surgery checklist >
Back to top >
About the Procedure
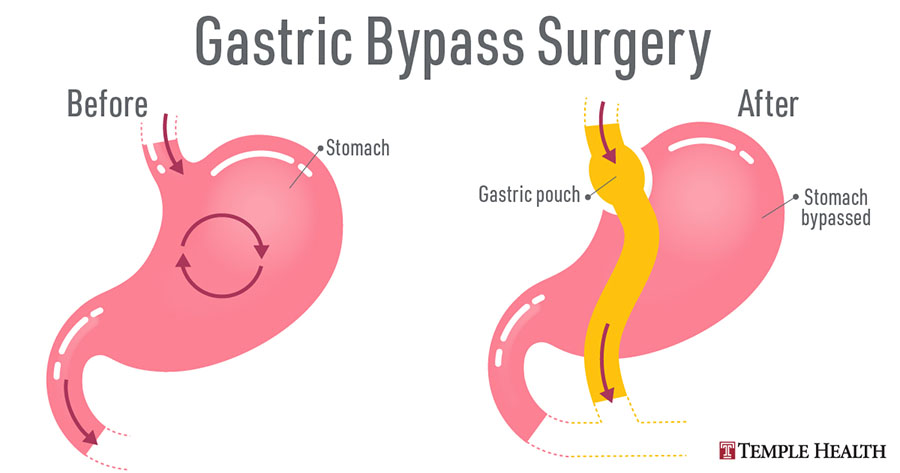
Gastric bypass surgically reduces your stomach size and reroutes the small intestines. It reduces how much you can eat and how many calories you absorb.
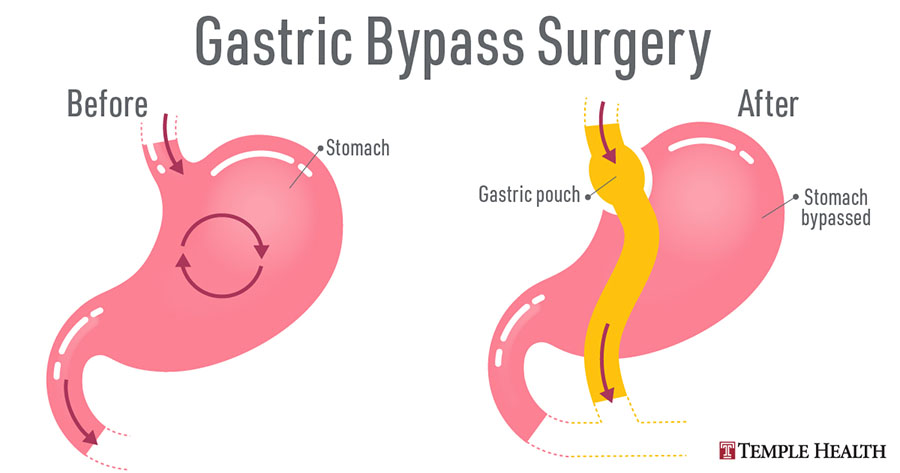
Roux-en-Y gastric bypass is performed by creating a small pouch from your stomach. Doctors then connect the pouch to your small intestine. This sends food past a large part of your stomach, reducing the overall functional volume.
If you have a gastric bypass, you’ll feel full after eating less food. This combined with the recommended nutrition plan will help you achieve successful weight loss. You’ll lose weight since you’re taking in fewer calories.
Surgery Approaches
Doctors refer to bariatric surgeries as restrictive or malabsorptive. Procedures generally involve one or both of these approaches:
- Restrictive – Restricts how much you eat by decreasing your stomach size
- Malabsorptive – Changes how you absorb calories and nutrients by changing your digestive-tract structure
Traditional vs Minimally Invasive Surgery
Roux-en-Y gastric bypass surgery is a traditional bypass surgery that involves creating a stomach pouch and surgically redirecting or bypassing your intestines.
With minimally invasive (laparoscopic) bariatric surgery such as gastric sleeve, the potential benefits include fewer incisions so that you have less discomfort, less scarring and an easier recovery.
Your surgeon will recommend the best treatment method for you.
Back to top >
Diet After Surgery – Week by Week
After the gastric bypass surgery, you’ll follow strict dietary guidelines that are essential to proper nutrition and healing. Avoid getting too full – especially while your newly created pouch heals. After that, keep portion sizes small to maintain weight loss. Your Temple Bariatric team will help you progress through these dietary phases based on your recovery process.
You progress through these diet phases: