What you'll learn on this page:
- Qualifications
- How to Prepare for Surgery
- About the Procedure
- Diet After Surgery – Week by Week
- Benefits and Risks
- An Experienced Team
Gastric sleeve, also referred to as sleeve gastrectomy, is a type of bariatric (weight-loss) surgery that treats obesity and other metabolic disorders such as diabetes, heart disease and stroke.
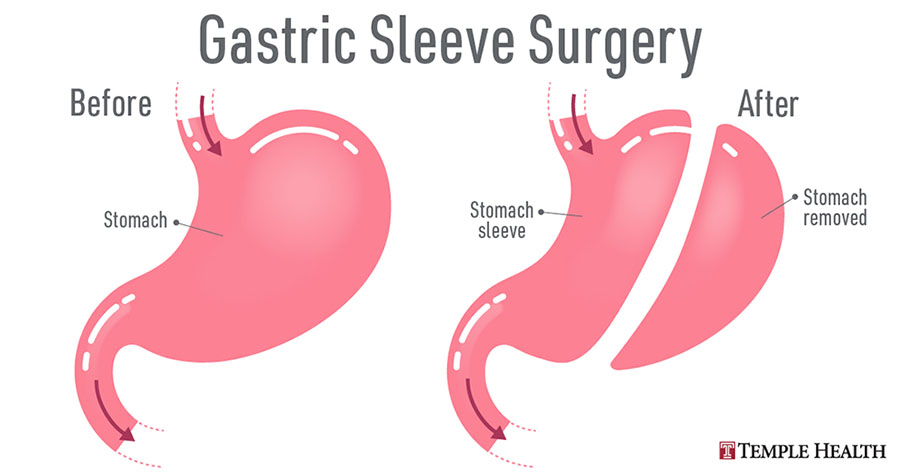
Gastric sleeve surgery is performed using tiny incisions to remove a portion of your stomach. This is known as a laparoscopic approach because your surgeon uses a small camera to guide the surgical instruments. Minimally invasive surgery such as gastric sleeve results in a faster recovery because the incisions are smaller and quicker to heal, with less pain than gastric bypass.
The procedure restricts what you can eat by surgically reducing your stomach size. It’s common to lose 60 to 70% of excess weight within a year or two after you have sleeve gastrectomy.
At Temple Health, weight-loss surgery is just one part of a lifelong health plan. If you qualify for a gastric sleeve procedure, our multidisciplinary team and motivating support groups will ensure you have all the support you need. We help you lose weight and keep the weight off.
Qualifications
Gastric sleeve may be an option for you if diet and exercise programs have not worked, and if you meet the following criteria:
-
Your body mass index (BMI) is over 40.
-
You have a BMI of 35 to 39.9 and have two or more obesity-related conditions metabolic syndrome such as high blood pressure, sleep apnea, diabetes or heart disease.
Check your BMI using our calculator: