What Is COPD?
COPD is a chronic inflammatory lung disease that prevents the lungs from getting enough air, making it very hard to breathe. Two of the most common types of COPD are chronic bronchitis and emphysema. It's most often caused by smoking cigarettes or other tobacco products, or long-term exposure to lung irritants, such as air pollution, chemicals or dust.
When a person has COPD, less air is able to flow into and out of the lungs because of one or more of the following:
- The walls of the airways in the lungs, known as bronchial tubes, become inflamed and thickened (known as chronic bronchitis).
- The walls between many of the tiny air sacs in the lungs are destroyed (known as emphysema).
- The air sacs and the airways in the lungs are less elastic.
- The airways in the lungs produce more mucus than normal, which can cause them to become clogged.
Stages of COPD
Doctors use staging to describe the severity of your COPD. Staging of COPD is one of the most important steps in diagnosis, and helps your doctor determine the best treatment plan for you. While COPD is a chronic disease with no cure, many treatments are available to help you breathe easier and have a better quality of life, at all stages.
To stage your COPD, you will meet with a specialist who will talk to you about your symptoms and schedule you for pulmonary (lung) testing. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) staging system is the most common method of staging COPD, and grades the severity of your COPD based on:
- Results from your pulmonary function test (PFT), a test that measures the amount of airflow going in and out of your lungs.
- Type and severity of your symptoms.
- How many times you have had moderate to severe flare-ups (also known as exacerbations).
- Whether you have other chronic diseases, in addition to COPD.
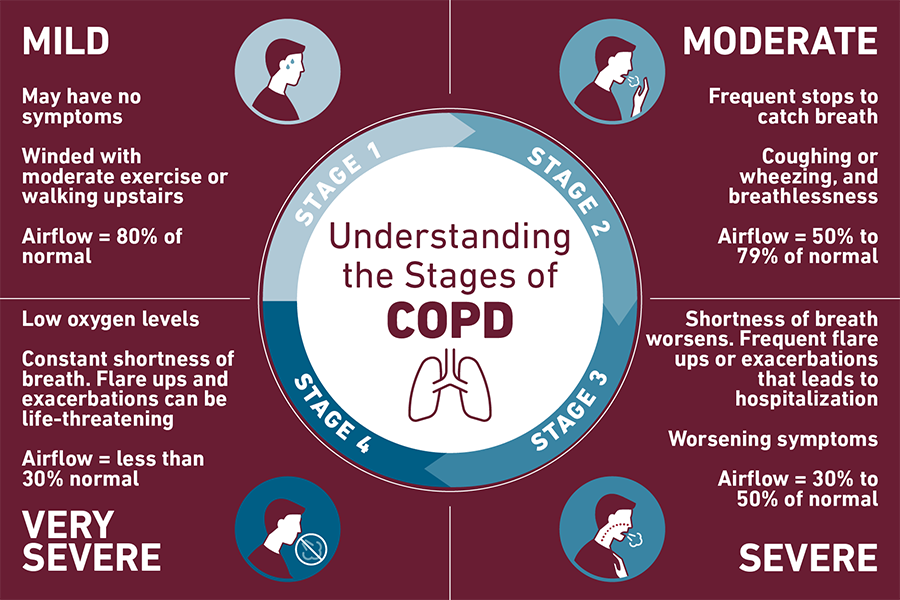
Your doctor assigns 1 of 4 stages to your COPD. These stages include:
Stage 1: Mild
You may have no symptoms, or you may get winded with moderate exercise or when walking upstairs. Your pulmonary function test indicates that your airflow is about 80% of normal.
Treatment at this stage may include lifestyle modification such as quitting smoking, taking certain medications and participating in pulmonary rehabilitation.
Stage 2: Moderate
You may need to stop and catch your breath when walking on level ground. You may complain of coughing or wheezing, and breathlessness. Your pulmonary function test indicates that your airflow is about 50% to 79% of normal.
Treatment options include medications, such as bronchodilators, anti-inflammatory medicines and antibiotics. You will also continue pulmonary rehabilitation to help you learn breathing techniques and lifestyle modifications that help you manage your symptoms.
Stage 3: Severe
Your shortness of breath is limiting your life and daily activities, with worsening symptoms. Your pulmonary function test indicates that your airflow is about 30% to 50% of normal. You may need additional tests at this stage to see how your lungs are functioning.
Treatments for stage 3 COPD include medications such as inhalers and bronchodilators as well as oxygen therapy and continued pulmonary rehabilitation. Flare-ups may be managed with corticosteroids and/or hospitalization.
Stage 4: Very Severe
Known as end-stage COPD, your oxygen levels are low due to lack of airflow. You will have difficulty catching your breath, even at rest. You may also have severe flare-ups causing frequent hospitalizations. These flare-ups may be life- threatening. Your pulmonary function test indicates that your airflow is less than 30% of normal.
Treatment options at stage 4 may include bronchoscopic lung volume reduction (BLVR) in addition to other medications mentioned in previous stages, or lung transplant.
Groupings Determine Risk of Flare-up
In addition to the four stages, doctors use groups to describe the risk of flare-up (also known as exacerbations). You may be placed into 1 of 4 groups — A, B, C or D. Your assigned group will depend on symptoms and how often you have flare-ups. As with stages, the 4 groups progress from mild to severe.
Group A patients have mild COPD symptoms and lowest risk of exacerbation, and Group D patients have severe symptoms and frequent exacerbation.
COPD clinical trials for all stages of COPD are ongoing. Clinical trials are research studies that aim to test or observe a medical, surgical, or behavioral intervention, and may give patients access to new and emerging therapies. Talk to your doctor to see if you qualify for enrollment.
Risk Factors
Risk factors for COPD include:
Smoking
Smoking cigarettes is the leading cause of COPD. Inhaling smoke from cigarettes damages the air sacs, airways and lining of your lungs. Other types of tobacco smoking — including pipes, cigars and water pipes — and smoking marijuana are also risk factors.
Environment
Long-term exposure to second-hand smoke and other lung irritants, such as air pollution, chemical fumes or dust also damage the lungs and can lead to COPD.
Genetics/Family History
Alpha-1 antitrypsin deficiency (AATD) is an inherited genetic condition where the liver does not produce enough of a protein called alpha-1 antitrypsin (AAT). AAT helps protect the lungs as part of a healthy immune system. 80% of people with AATD develop COPD.
Age
It takes several years to develop COPD. Although it can develop at an earlier age, many people start to notice symptoms around the age of 40.
Prevention
Because smoking is the number one cause of COPD, quitting smoking is the best way to prevent it. Even if you have been diagnosed already and currently smoke, you can improve your lung function and slow the progression of COPD by quitting smoking. Within 2 to 3 months of quitting, your lung function will start to improve. And within the first 9 months, you should notice improvement in symptoms of cough and shortness of breath.
If you’ve tried and failed to quit smoking before, consider joining our Smoking Cessation Program. Research shows support groups increase your chances of long-term success.
If possible, try to avoid long-term exposure to lung irritants that can also contribute to COPD, such as:
- Air pollution
- Chemicals
- Dust
- Second-hand smoke
Choose the Temple Lung Center
Helping patients breathe easier and enjoy a higher quality of life are our main goals. Our widely respected COPD specialists work to achieve these goals by offering innovative treatment options and performing cutting-edge research. It’s this combination that has led Temple’s COPD Program to be recognized as a worldwide leader in caring for this complex disease.
Our Team
The Temple Lung Center is led by Gerard Criner, MD, an international leader in pulmonary care, and is staffed by many physicians and surgeons who are recognized as “Top Docs” by respected publications and organizations. These specialists are also renowned researchers who are developing and testing new treatments for COPD.
The experience of having COPD is different for everyone. Those with mild disease may require monitoring and lifestyle modifications, while people in the more severe stages of the disease often need medical, emotional and social support to help them overcome the daily challenges of living with COPD.
Learn more about COPD treatment options for Temple patients >
Your treatment plan may change over time as your disease progresses. Because of this, Temple coordinates COPD care between pulmonary physicians and a team of highly trained nurses, respiratory therapists and other medical professionals with years of experience treating people with COPD and other complex lung diseases.
This team approach allows for:
- Open communication between team members and patients
- Access to specialists and programs that may help improve quality of life
- Personalized approach that helps patients feel supported
Ready for an Appointment?
If you're experiencing signs or symptoms of COPD, schedule an appointment or call 800-TEMPLE-MED (800-836-7536) today.
Learn more about our doctors and care team who diagnose and treat COPD.



